Saint-Louis Hospital
To understand how respiratory-borne pathogens spread and prevent the transmission of viruses among immunocompromised patients, teams from the Saint-Louis University Hospital have joined forces with Dassault Systèmes to carry out a study of airflow simulations in the dialysis department. Through its Virtual Twin as a Service approach, the company built a virtual twin of the dialysis unit to be able to identify a concentration of airborne particles and raise the awareness of health professionals.
Preventing respiratory transmission of viruses in hospitals
When patients come to Saint-Louis Hospital – APHP in Paris, the last thing they want is to pick up a virus during their stay. For the 50 people receiving dialysis every week, extra precautions are crucial. Patients suffering from kidney failure are immunocompromised and more susceptible to infections. Every other day, they must attend the dialysis unit for treatment, sitting alongside other patients in one room. Aside from wearing masks and maintaining good hand hygiene, the hospital’s infection prevention and control team, known as ESPRI (Equipe de surveillance et de prévention du risque infectieux), wanted to see what else could be done to avoid respiratory transmission of viruses.
“The dialysis unit of Saint-Louis Hospital is an open space simultaneously treating up to nine patients,” said Dr Fabien Métivier, a nephrologist at Saint-Louis. “We were struggling to understand airborne transmission of pathogens among these fragile patients. Dr Guillaume Mellon suggested to carry out an air flow simulation study.”
As part of his role, Mellon is responsible for monitoring everything related to infection risk transmission in the hospital. He and the ESPRI team joined forces with the virology department. Together, they began an investigation within the dialysis ward, comparing the levels of virus particles in the air at different times of day and at night when the service was closed.
The team took vacuum air samples from different parts of the room to see if patients were exposed to higher levels of virus concentration depending on where they were situated. The team discovered that during the day, virus particles were circulating despite bio-cleaning between sessions. At night, hardly any particles were detected.
“We realized that the results varied depending on the location of the different samples,” Mellon said. “One of the samples came back with a 56% positivity rate versus 7% for another one at the other end of the room. How could this be explained?”
The team suspected there may be an imbalance in the ventilation network. It wanted to find out more and carry out an airflow simulation study.
With Dassault Systèmes, thanks to augmented reality, an innovative educational tool, we have been able to reveal the invisible.
Trusting in proven expertise
Mellon reached out to Dassault Systèmes, aware that the company already had experience working on similar projects with other hospitals. Of particular importance to Saint-Louis was the fact it was possible to outsource all necessary modeling and simulation work to Dassault Systèmes through its Virtual Twin as a Service (VTaaS) approach.
“Dassault Systèmes is expert in flow modelization and knew the issues we faced as they had already worked on projects at the Salpêtrière, Bichat and Avicenne hospitals in Paris," he said. "We didn’t need much convincing. We trusted them straight away.”
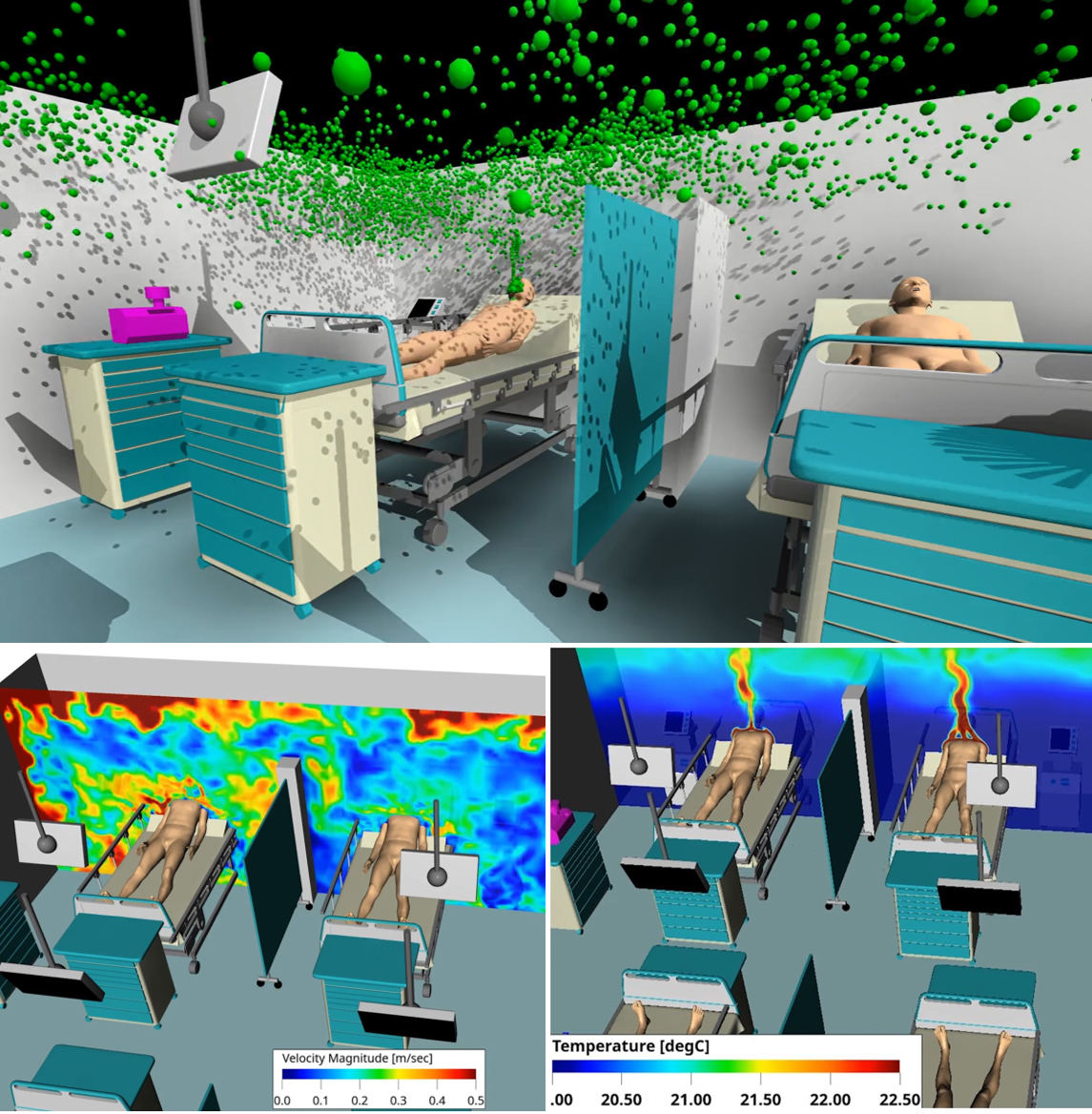
In the first meeting, Dassault Systèmes guided Mellon and the team to check the entire ventilation system, examining the airflow in the room, including the air inlet and outlet. The measurements revealed there was insufficient airflow. What followed over the next few months was an extensive study into airborne propagation of pathogens within the dialysis department. Through the VTaaS approach, Dassault Systèmes’ experts created an accurate, full-scale virtual twin of the room. They simulated particle contamination and tested different scenarios and setups within the space to improve ventilation before presenting their findings. All work have been carried out on the 3DEXPERIENCE® platform on cloud.
“Our interactions were very rich and dynamic,” Mellon said. “The Dassault Systèmes team was proactive and came up with proposals to go further. And the 3DEXPERIENCE platform on cloud was very practical for sharing information. The entire experience exceeded my expectations.”

Airflow simulations highlight virus spread
The success of the project came down to Dassault Systèmes’ ability to merge the physical and virtual worlds. To create a virtual twin of the dialysis unit, the company worked with building blueprints, coupled with a 3D scan of the room made on-site using the HomeByMe mobile app to check for any discrepancies.
The team then performed airflow simulations using SIMULIA Fluids solutions on the 3DEXPERIENCE platform to accurately visualize and predict the transmission of respiratory and viral particles through the air. The initial results revealed that specific areas of the room were lacking airflow, allowing virus particles to cluster. Different scenarios have then been simulated to improve ventilation, taking into account the location of medical equipment and patients in the room.
“The solution allowed us to visualize the production of respiratory particles, follow their trajectory, and see that a patient at one end of a 250-meter squared room can contaminate a patient at the other end of the room with their respiratory secretions,” Mellon said.
“Dassault Systèmes helped us reveal the invisible in all manner of different scenarios: with and without a mask, when patients were breathing in and out, according to different air flow rates and whether the doors were open or closed,” added Nathalie Osinski, nurse manager at ESPRI.
Hands-on experience with augmented reality
Going one step further in the project, Dassault Systèmes' teams have developed an augmented reality experience to present their findings and recommendations. They invited key stakeholders in the hospital to gather in the dialysis department and see the results for themselves. Attendees were given tablets so they could view the virtual simulations within the real-life setting to see exactly how virus particles were transmitted.
“When the augmented reality simulation was revealed, everyone was captivated,” Osinski said. “Each person had a tablet in their hands, could walk to each bed and see how the virus particles circulated in the room depending on where they stood. We could see the particles’ direction of travel towards the ceiling and into the air vents.”
"It's a unique experience in a hospital and an incredibly innovative educational tool that enabled us to make health professionals aware of respiratory cross-transmission risks in the hospital,” Mellon added.
Saint-Louis hospital has since taken proactive measures to improve ventilation in the dialysis department. It has also reviewed its policies so it now keeps doors closed, for example, and reconsidered how it organizes its clinics to protect higher risk patients.
“Augmented reality provided us with very visual information on the dissemination of respiratory particles,” Mellon said. “In a very practical way, I now know where a dialysis patient with flu has to be placed in the room to prevent contaminating all the other patients.”
Mellon and his team then carried out a follow-up study to ensure they’d effectively addressed the issue and successfully reduced the potential for virus transmission. The virological results had been normalized and this variation or hyper concentration of the virus in specific parts of the dialysis room no longer exists.
“It made us think that we should take advantage of this type of study every time there is an infectious risk in a hospital department,” Métivier added.

Innovation in patient care
Mellon and the team at Saint-Louis are excited about how else technological innovation can be applied in hospitals in general to protect the most vulnerable patients better.
“We are at a turning point in terms of new technologies,” he said. “Some viruses could be less dangerous for ordinary people, but critical for hematology patients. Now it’s possible to detect them and identify ways to prevent them from spreading. This could really help to reduce the risk of infection. It would be really interesting to develop a training project that could be used by all the infection prevention and control teams in French hospitals.”
Based on the success of this VTaaS approach, another unit within Saint-Louis is already working with Dassault Systèmes on a similar initiative around daily patient care and infection prevention. Partnering with Dassault Systèmes allows the hospital to more easily access emerging technologies without having to invest in them upfront or develop new IT capabilities in house. It also helps to boost the hospital’s reputation as a leading health provider and encourages broader transformation across the sector through new ideas and tools.
“These types of partnerships are essential, especially when designing new hospitals and departments as they can help to determine the optimal location of air vents, beds and how patients should be positioned in the room,” Osinski said. “We have so much to learn about air flows and how they affect healthcare settings and patient care.”

Focus on Saint-Louis Hospital AP-HP
Saint-Louis is a quaternary care academic public hospital, part of the Assistance Public-Hôpitaux de Paris (AP-HP) Group. The hospital specializes in a large number of medical and surgical disciplines, including hematology, cancer and dermatology, as well as infectious and tropical diseases, and inflammatory diseases.
For more information: https://hopital-saintlouis.aphp.fr

